Risk vs. Vulnerability — The Real Reason Traditional Predictive Analytics Will Always Fall Short
By Dr. John Showalter, MD, MSIS, Chief Product Officer at Jvion

Risk and vulnerability seem like synonyms. In the context of the pandemic, you might say a patient is at risk for Covid-19, or you might say the patient is vulnerable to Covid-19. Same thing right? However, understanding the difference between the two concepts can have big implications for how providers respond and protect their patients from harm.
What is Risk?
Providers are more than familiar with risk: their payment models are increasingly risk-based arrangements, and there are countless software tools available that assign risk scores to patients to help providers focus their attention on patients at the greatest risk. By reducing patients’ risk, providers can prevent injury or disease and ultimately save money under these risk-based payment models.
In this common understanding of risk, risk is a linear distinction. Somebody is either at risk, not at risk, or somewhere in the grey area between the two. But importantly, risk doesn’t tell you why somebody is at risk, or even more importantly, what you can do about it.
This is where vulnerability comes into play.
Understanding Vulnerability
In the software world, a vulnerability is a gap in the software’s protections that exposes the software to a threat, like a hacker. When vulnerabilities are detected, they are patched as soon as possible. It works the same way in healthcare: a vulnerability is a gap in your efforts to protect your patients from harm. And like in software, vulnerabilities can be addressed.
In this way, vulnerability can be thought of as the part of risk that you can change. Some elements of risk — like chronic conditions, age, or genetics, for example — are unavoidable. On the other hand, health systems can take steps to address vulnerabilities and, as a result, reduce patients’ risk for avoidable harm and hospital utilization.
Vulnerabilities come in many forms. They can be emotional or cognitive vulnerabilities, for instance if a patient suffers from depression and struggles to find the motivation to eat healthy, exercise, or take their medication. Or, they can be social and economic vulnerabilities — also known as social determinants of health (SDOH) — for example if patients can’t afford to eat healthy foods or pay for their prescriptions, or if they don’t live near a pharmacy or a food bank that can help them.

Vulnerability and the Pandemic
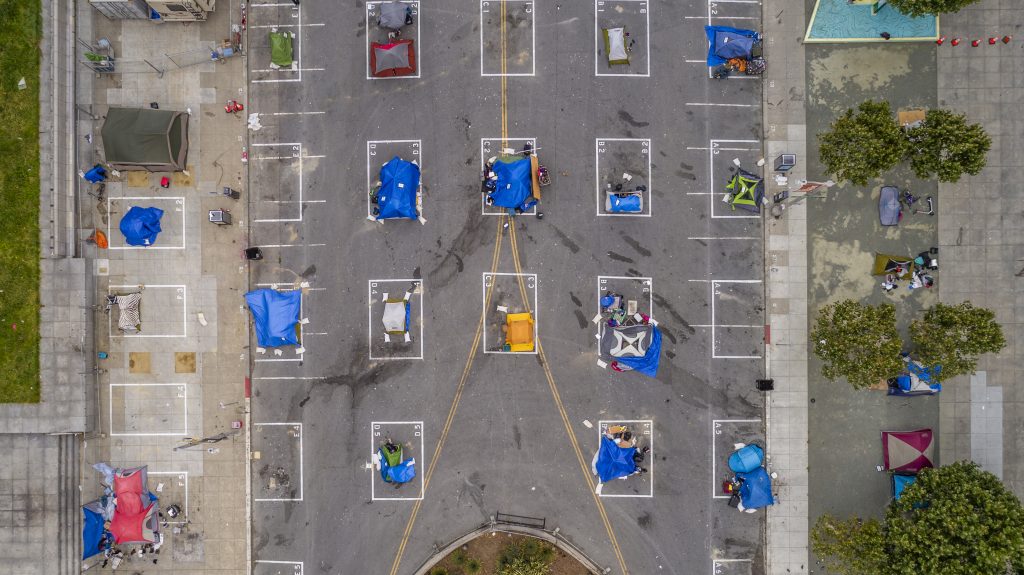
The pandemic has brought the impact of vulnerability into sharp focus. Across the country, the people who are infected, hospitalized, and dying the most are those with the most vulnerability: people working low-wage frontline jobs, the homeless, those with chronic exposure to air pollution, those in minority communities long deprived of equal healthcare resources, and those in underserved rural communities as well.
At Jvion, we believe that addressing vulnerability is the key to improving health outcomes, raising the quality of care, and lowering health costs. It’s why we created the COVID Community Vulnerability Map and Patient Vulnerability Lists to help hospitals and health systems proactively take steps to protect their most vulnerable patients during the pandemic.
Applying the insights from these tools could mean simply educating vulnerable patients about their unique risks, establishing mobile testing sites in vulnerable communities to catch illness early, or helping unemployed or low-income patients enroll in Medicaid or other financial benefits so they can afford their care should they need it.
How to Mitigate Vulnerabilities
In any case, providers can mitigate the vulnerabilities of their patient population — but only if they know they exist. A risk score alone won’t show you the socioeconomic and behavioral vulnerabilities that are driving risk. This context is critical to helping patients stay healthy, but more often than not, it is completely invisible to providers.
For these deeper insights, you could take the time you don’t have to ask each of your patients dozens of questions. Or, you could use readily available data — from sources like the Census, USDA, EPA, HUD, credit reporting agencies and other consumer data aggregators — that point to external behavioral, environmental, or socioeconomic vulnerabilities. But to draw the relevant insights from this data, and present it in a way you can use, you need clinical AI.
Our clinical AI, the Jvion CORE™, looks at over 4,500 risk factors, including clinical, socioeconomic, environmental and behavioral factors, to give providers and health plans a comprehensive view of vulnerability in their patient population. Perhaps more importantly, it goes a step further and provides recommendations to address each patients’ unique vulnerabilities, saving providers time and energy.
These vulnerability insights make a real difference not only for patients but also for providers. The Center for Cancer and Blood Disorders in Texas, for example, saved over $3 million in six months, raised their quality scores, and substantially reduced ER visits and hospitalizations. Meanwhile, a provider-sponsored health plan in the MidWest reduced admissions by 63%. For more case studies, check out our insights and resources page.